Further to presentation of the e-Ageing project orally and in abstract form (detailed below), the full manuscript describing the development […]


Further to presentation of the e-Ageing project orally and in abstract form (detailed below), the full manuscript describing the development […]
Your general observation is that Mrs Browning appears to be a very alert, independent and capable elderly woman. She is cheery, well presented and easily mobile.
Height: 178cms
Weight: 67.5kg (an increase of 1.5 kg)
Please move your cursor over Mrs Browning as if you were examining her. You must complete the examination before you go on.

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up
Mrs Cloverdale scores 7/15 on the GDS, indicating that psychological review is recommended. You discuss the result with Mrs Cloverdale and suggest the option of referral to a psychologist. She is happy with this plan and you indicate you will follow this up at review.

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up
Fortunately, Mrs Wood has a normal CT scan.


Time's up
Click here to see Dr Zheng’s MMSE result
Dr Zheng was disoriented. He was able to repeat three words immediately, but was able to recall only one. He spelled ‘world’ backwards correctly for two letters, but missed the last three. He was unable to read commands correctly but followed verbal commands (by interpreter). He could write a simple sentence with assistance, and incorrectly copied the intersecting pentagons.
Dr Zheng scored 15/30 on his MMSE. This is consistent with progression of his Alzheimer’s disease.

Time's up

Time's up

Time's up

Time's up
Common Differentials: the DDD CHART
Feature | Dementia | Delirium | Depression |
Onset | Gradual | Abrupt (hours to weeks) | Either |
Prognosis | Irreversible | Reversible | Variable |
Course | Progressive | Worse in p.m. | Worse in a.m. |
Attention | Normal | Impaired | Variable |
Memory | Impaired recent and remote | Impaired recent and immediate | Selective impairment |
Perception | Normal | Impaired | Normal |
Psychomotor behaviour | Normal | Very active / Unusally quiet and still | Retardation / agitation |
From: Resnick.B. Restorative Care Nursing for Older Adults: A Guide for All Care, 2004,

Time's up

Time's up
MRI is a structural neuro-imaging method that provides images of the brain and other anatomical structures. Some studies using MRI have demonstrated that medial temporal lobe (MTL) atrophy can be predictive of Dementia Alzheimer’s Type (DAT) and that has been associated with neuropsychological and post-mortem data. MRI may assist in the diagnosis of DAT.
An MRI may be obtained if it is suspected that the patient has dementia, however MRI is not required to make a diagnosis of dementia
Dr Zheng’s brain MRI is provided below:
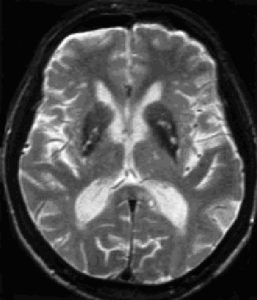
Brain imaging indicates volume loss, consistent with dementia. No evidence of masses or vascular disease.
CT is a relatively inexpensive, quick and non-invasive scan that produces images of brain structures such as the grey matter, white matter, cerebrospinal fluid cavities and blood vessels. These images may also reveal abnormalities such as tumours, strokes, and head injuries. The role of CT imaging in the diagnosis of dementia is primarily one of exclusion. Evidence based guidelines suggest that structural neuro-imaging with either CT or MRI scan is appropriate in the routine initial evaluation of patients with dementia.


Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up

Time's up
The physiotherapy consult finds her Berg balance scale is 27/56. She has difficulty transferring, turning, reaching and balancing on one foot. The physio recommends some lower limb strengthening and gait exercises and some mild exercises to help rebuild her wasted quadriceps. It is important that Mrs Scott maintains participation in physical activity, in order to maintain muscle strength and joint range of movement and to improve her balance.
The physiotherapist prescribed specific mobility exercises (including stretches in prone lying) and specific strengthening exercises for hands and her leg extensors (which can be performed as a home program).

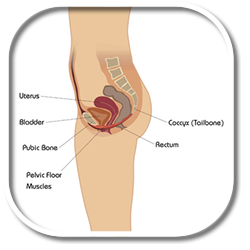
The physiotherapist uses models of anatomy to explain the physiology of voiding and bladder control problems. To help reduce stress incontinence, Mrs Scott’s pelvic floor muscles are assessed and found to be lax. Mrs Scott has been performing the exercises prescribed by the NCA, so the physiotherapist checks her technique to ensure she is doing them correctly. Further advice was needed to refine technique. Mrs Scott is aware that she needs to do these exercises at least 5 times per day, every day in order to recondition her pelvic floor.
To further address urge incontinence Mrs Scott will perform timed voiding, as advised by the NCA.

Time's up
Mr Scott looks well. His affect is reactive but be appears to be slightly anxious.
Height: 184cms
Weight: 98kg (which has remained constant)
Please move your cursor over Mr Scott as if you were examining him. You must complete the examination before you go on.
Hover over or click on a body region to view examination findings
Click to keep this information visible

Time's up
Respite Care is short term care to “give carers a break”. This can be provided, in home for a few hours, or the care recipient may move into a residential facility for a number of weeks
Other Palliative Care Resources
Palliative Care Knowledge Network: an online resource which provides information about palliative care: www.caresearch.com.au
Palliative Care Australia: the national peak body for palliative care in. www.palliativecare.org.au
Advice on how to discuss palliative care with the patient and their family at: https://www.caresearch.com.au
or
Clinical practice guidelines for communicating prognosis and end-of-life issues with adults in the advanced stages of a life-limiting illness, and their caregivers https://www.mja.com.au/public/issues/186_12_180607/cla11246_fm.html
Physical Measures
Wt=90.4kg
Biochemistry
Urea, Creatinine & Electrolytes – normal
Full Blood Count – normal
BGL measured on ward daily
0600hrs fasting: 5.1-6.5 mmol/L
1230hrs before lunch: 6.0-7.0 mmol/L
1800hrs before dinner: 5.3-6.7 mmol/L
2000hrs: 8.3-9.7 mmol/L
Like many patients Mr. Tanner has quite a number of issues to consider in planning to return to community living. Some of these issues will include;
All of these sorts of issues will be discussed with Mr Tanner and with the family in order to make sure that discharge is appropriate.
We also need to check with Mrs Tanner and make sure that she has an understanding of what has occurred so far, and potentially the long term implications are.
Issues such as;
All of these sorts of issues will need to be looked at.
Multidisciplinary Pain Management Programs have an increasing evidence-base to support their use in reducing suffering and pain perception. The success of these programs is in their adoption of a Cognitive Behavioural approach to management.
Pain Management Programs have the capacity to improve the patient’s quality of life, reduce suffering and distress and provide a more satisfying daily lifestyle. They are not designed to eliminate pain or provide the patient with a cure.
Wt=91kg
Biochemistry
Urea, Creatinine & Electrolytes – normal
Full Blood Count – normal
BGL measured on ward daily
0600hrs fasting: 5.1-6.5 mmol/L
1230hrs before lunch: 6.0-7.0 mmol/L
1800hrs before dinner: 5.3-6.7 mmol/L
2000hrs: 8.3-9.7 mmol/L
Dysphasia is an acquired communication disorder that results from damage to the language areas of the brain. It can affect the expression (expressive dysphasia) and comprehension (receptive dysphasia) of language, including reading and writing skills. Expressive dysphasia can be classified into fluent and non-fluent forms. Individuals with non fluent dysphasia tend to have reduced rate of speech, effortful articulation and word finding difficulties.
A speech pathologist’s role in stroke management can be both in areas of communication and swallowing.
First, starting with swallowing, around 27-50% of all acute stroke patients experience dysphagia or swallowing difficulties. Dysphagia results in decrease in nutrition and hydration, greater risk of aspiration pneumonia, increased length of hospitalization, illness, and in some cases even death.
Speech pathology intervention focuses on assessment, and management of swallowing and eating difficulties following a stroke.
So, when a patient first presents to me, after they’ve had a stroke, I need to establish;
In those such cases, I need to liaise with the dietician, and refer to their expertise, and collaborate together with them to effectively manage a nasogastric regime.
There is also a role in dysphagia for education of patient, family, and the stroke team in regards to safe swallowing strategies as well as the continuous monitoring and reviewing of the patient, to monitor progress, or also the regression.
A stroke can also affect communication skills, resulting in a disability due to dysphasia, which occurs in a frequency of around 21-38% of all acute strokes, and/or dyspraxia and dysarthria which occur in incidence of 20-30%.
Communication impairment can also be secondary to cognitive problems, such as decreased concentration, attention, increased tiredness, memory, and problem solving deficits. Speech pathology provides specialized assessment, therapy, and advice regarding the best way to help a patient who has a communication problem.
The impact on a patient who does have a communication problem can be a very isolating experience for them. There is a lack of power because they are not able to get their basic needs and wants met because they aren’t able to communicate those. There is anxiety, the patient is also unable to participate fully in the recovery and rehabilitation process. There is also impact upon all allied health nursing and medical staff. There is frustration within staff members because they are unsure in how to engage the patient. There is increased time needed to actually communicate effectively. There’s also the difficulty in building up rapport and developing the whole therapeutic alliance.
So, a speech pathologist works to establish; how is a patient able to express their basic needs and wants? Can the patient actually understand? And then you can establish a basic communication system which allows the patient to participate in recovery, for them to be able to state their wants and needs, be provided with some sort of choice.
Sometimes, if they are unable to speak or express what they want verbally, we can resort to alternative communication systems, such as communication boards.
A speech pathologist’s role also incorporates education again; the provision of information to the patient, the family as well as the stroke team regarding the best suited mode of communication for the patient, as well as ongoing communication therapy for that patient.
The role of occupational therapy in stroke is two-fold. We can treat people as a rehab candidate as an inpatient, and also have a big role in the discharge planning process.
We treat people by looking at their abilities to complete their desired activities, whether that’s self-care, occupation and leisure.
As an inpatient in rehab, OT’s breakdown activities into smaller parts to ensure that a person can perform affectively in their desired tasks.
The sub-components are;
How the patient moves (so that’s their motor area) and we concentrate specifically on the person’s upper limb as this has most to do with their function in every day life.
We also assess sensation, which is their awareness of their body.
We also assess their vision, which is obviously their eyesight and to make sure that they don’t have any visual field deficits.
Also perception, how people make sense of their incoming information.
We also assess and treat cognition, which is how the person plans to react to that incoming information.
We can also look at the person’s mood and behaviour, as potentially, after stroke, people have a lot of adjustment problems.
We assess these components and treat these areas incorporating them in function so to ensure as well that the patient can actually achieve the desired outcome.
The main problem for Mr. Tanner, we would envisage, is first of all positioning. We would need to liaise with the nursing staff and physiotherapists to ensure that Mr Tanner has correct positioning in both bed and chair, as this may compromise his rehab.
We would also expect him to have reduced sensation and movement in his side contra-lateral to his lesion.
We also suspect that he may have an apraxia, which is a motor planning problem or it’s the idea that he has lost the concept of particular activities.
Lastly, we play a major role in discharge planning. So we need to assess whether the patients environment at home is suitable for him to return to. We would need to take him on a home visit and check for rails and equipment, and we would supply those prior to discharge.
The role of the Physiotherapist is to assess and treat
The TACS patient will undergo assessment initially by the medical team to reverse the damage; nursing staff will monitor and position the patient.
Points to consider
Usually, a lesion of this size means the rehabilitation process in hospital may take as long as 3 months and will require regular team meetings and goal setting with constant communication between all disciplines and family.
Acute hospital measures
Wt=92kg
Rehab admission measures
Wt=91.6kg
Ht=170cm
BMI=31.7kg/m2 (30.0-34.9 obese class I)
Waist=130cm (>102 greatly increased health risk)
Blood pressure 140/85 (reported by doctor) borderline
Biochemistry
Urea, Creatinine & Electrolytes – normal
Full Blood Count – normal
Lipids – Chol=5.3 (<5.5) LDL=4.0(<3.0) HDL=1.1(>1.0) TG=2.5 (<2.0)mmol/L
HbA1c = 6.9% (6.0-7.0% good control) Fasting BGL=5.8 (3.0-5.4)mmol/L
Urinary Microablumin and microalbumin/creatinine ratio – normal
BGL measured on ward daily
0600hrs fasting: 5.1-6.5mmol/L
1230hrs before lunch: 6.0-7.0mmol/L
1800hrs before dinner: 5.3-6.7mmol/L
2000hrs: 8.3-9.7mmol/L
A depressed individual may require management of their depression before engaging in active rehabilitation. Depression impacts upon how a patient processes information. Negative thinking makes it difficult to find positive memories to use in the process of developing new goals. Depressed patients also have difficulty in developing concepts for a positive future. The practical implications for this in rehabilitation is that goal-setting may be unsuccessful without targetting depression first.
The Functional Independence Measure (FIM) is an outcome measure of the severity of disability for an inpatient rehabilitation setting. It rates 18 activities of daily living on a 7- point scale ranging from fully dependent (1) to independent with no aids (7). Improvements in functional status can easily be reviewed over time including at discharge and follow-up.
The Barthel Index establishes a patient’s degree of independence in activities of daily living. Scoring is done either by direct observation or by asking the patient, nursing staff or family members.
The primary goal of rehabilitation is to restore the individual to their greatest potential and maximise independence.
Rehabilitation is concerned not only with physical recovery but also with reintegration of the person into the community. The central aspect of rehabilitation is provision of a coordinated program by a specialised, interdisciplinary team of health professionals that is developed in consultation with the patient and their family/caregiver. Successful rehabilitation involves adopting a broader perspective that includes physical, social and psychological functioning.
Other factors that influence successful rehabilitation include:

Time's up

Time's up
It is commonly thought that to maintain physiologic homeostasis may help to minimise the brain damage due to stroke. Thus we generally try to avoid hyperglycaemia.
Many patients with stroke will have hyperglycaemia so it is a common problem. Hyperglycaemia is an independent predictor of poor outcome, but the GIST trial – a randomised controlled trial of glucose/potassium/insulin infusion compared to normal saline, for tight blood glucose control – was negative. Unfortunately, the trial was underpowered so some uncertainly persists.
Prevention of Deep Venous Thrombosis is an important component of care in the stroke unit.
Stroke unit care uses a range of approaches to try and reduce the risk of venous thrombosis including a focus on early mobilisation, and maintenance of adequate hydration.
We use a range of prophylactic therapies including physical compression stockings.
The benefits and risks of these need to be carefully considered, and further data are awaited.
We also use pharmacotherapy, especially unfractionated and low molecular subcutaneous heparin to try and reduce the risk of deep venous thrombosis.
Again, it’s important to weigh the risks and benefits of therapy as stroke patients are often at high risk of bleeding complications.
Hypertension is a significant issue with stroke for two reasons. Firstly, hypertension is the most important cause of stroke in our community and treatment of hypertension prior to stroke can be expected to reduce the patient’s risk of stroke, and as such one should always consider that.
But in the setting of secondary hypertension, that is in post stroke, as in this scenario, treatment of hypertension can be a little tricky at times. Often patients will have a markedly elevated blood pressure following stroke due to the activation of the sympathetic and cortisol based mechanisms such that their blood pressure will often be elevated in the region of 170-200mm systolic.
As you’ll be well aware, the brain has autoregulation and as such during this time, interfering with this autoregulation with aggressive blood pressure lowering may lead to actually increased risk of recurrent infarction and extension of the infarct that has already happened.
As such, when you are called to manage or asked to manage hypertension after stroke, once you consider that the blood pressure is 180 systolic it’s certainly probably safe and certainly don’t need acute management.
Blood pressures from 180 to just over 200 may need some cautious management with gradual blood pressure lowering agents. Whereas blood pressures beyond 220mmH certainly need to be acutely lowered, but again very cautiously, only lowering the blood pressure by perhaps 10-15% in the initial phase and not more than 25% over the next few days.
In terms of choice of medication for those without severe hypertension it has been well shown that ACE inhibitors plus diuretics as well as angiotensin receptor blockers are very safe medications for this indication.
For those with accelerated hypertension, that is blood pressure more than 220mm systolic and/or patients who have complications in their hypertension (such as headache, impaired consciousness or falling renal function), then perhaps a more aggressive strategy is warranted, but cautious lowering of blood pressure with an intravenous agent such as a nitrate or perhaps an intravenous dose of beta blocker may be effective.
It’s important to remember that treating hypertension is a lifelong experience rather than necessarily something that should be done in the first few days
No, the patient can’t just go to a rehab ward. Care on a stroke unit is the most effective way of treating stroke and improves both morbidity and mortality. A stroke unit is usually in a dedicated area of the hospital, where a specialized team looks after stroke patients. A stroke unit aims to promote recovery and independence in activities of daily living.
There is good evidence proving that stroke units reduce death, dependency and institutional care, without having adverse outcomes such as increased length of hospitalization. These benefits have been found to be independent of factors such as age, or the severity of the stroke.
For a more in-depth read of research that has been conducted thus far in regards to stroke units, begin by reading the findings of the stroke unit trials collaboration, who published their findings in the British Medical Journal in 1997, volume 314, page 1151.
There are several models of care, which may be called ‘stroke units’. Some are predominantly acute, or are rehabilitation units. Combined are comprehensive units providing both acute and rehab care. The evidence is clearest from these comprehensive units which follow a patient’s journey, right from the acute phase through to the rehab phase. In a comprehensive stroke unit, a specialized, multidisciplinary team provides a coordinated program that includes individual assessment, treatment, regular reviews, discharge planning, and follow-up.
A stroke may have left a person with a variety of physical complications ranging from problems with swallowing, continence, communication, and mobility. A stroke can also affect someone’s perception and cognitive skills. There are also psychological and emotional changes that can occur which may be quite difficult to cope with. Other changes which can also occur include depression, tiredness, memory problems, loss of concentration, personality changes, irritability and aggression. Therefore, effective rehabilitation provided through a stroke unit relies on a coordinated, multidisciplinary team approach.
There are mobile units which function in some centres. However, these are thought to be a less effective form of specialized stroke care. Now, for further bedtime reading in reference to stroke unit care, you can refer to the National Stroke Guidelines which can be found via the web, www.strokefoundation.com.au or you can also refer to a journal article by Peter Langhorne, which can be found in the Journal of Age and Ageing, published in 2001. This article can be found in volume 31, page 365.
Mr Tanner was offered endovascular thrombectomy and concurrent thrombolysis.
Click on the needle to see how he fared.
Great choice! Mr Tanner has endovascular thrombectomy and concurrent TPA within 2.5 hours of stroke onset. Within 15 minutes he is no longer aphasic, although his speech is still slow with some evidence of expressive dysphasia. His left arm weakness remains, but his left leg is much improved!
Thrombolysis has been used successfully in myocardial infarction for 20 years and has been shown to improve morbidity. In stroke patients it also works by acting as a plasminogen activator, which helps break up the fibrin rich clots which can cause strokes.
More recently, endovascular thrombectomy, in addition to intravenous thrombolysis within 4.5 hours (when eligible), has become the recommended line of treatment for acute stroke patients with large artery occlusions, up to 6 hours after symptom onset.
Neither of the combined therapies should prevent the initiation of the other, provided there are no contraindications to proceed. Intracranial vessel occlusion should be diagnosed with non-invasive imaging wherever possible, before considering treatment with endovascular thrombectomy. Patients with radiological signs of large infarcts (using the ASPECTS score), may be unsuitable for thrombectomy.
There can be an increased risk of cerebral haemorrhage with thrombolysis, so contraindications such as severe uncontrolled hypertension, direct thrombin inhibitors, acute intracranial hemorrhage, thrombocytopenia and coagulopathy, must be considered before proceeding.
Endovascular thrombectomy should be performed by an experienced neurointerventionalist who meets national and/or international requirements.
Urgent CT is mandatory to look for evidence of haemorrhage.
It’s also important to look for signs of stroke mimics (such as other space occupying lesions).
Early subtle signs of ischaemia may also be present on early CT and these include changes such as sulcal effacement.
It’s important to remember that if there are clear signs of ischaemic change, than the time of onset needs to be carefully re-checked, as the stroke may be older than initially thought.
TAC – Total Anterior Circulation
ALL of:
*epidemiological data suggest 1 year mortality to be 60%, with 36% of those surviving being functionally dependant.
PAC – Partial Anterior Circulation
Either:
*epidemiological data suggest 1 year mortality to be 16%, with 29% of those surviving being functionally dependent.
LAC – Lacunar
*epidemiological data suggest 1 year mortality to be 11%, with 28% of those surviving being functionally dependent.
POC – Posterior Circulation
Any of:
*epidemiological data suggest 1 year mortality to be 19%, with 19% of those surviving being functionally dependant.
Clinical classification systems (like the TACS, PACS, LOCS and LACS system) are useful in enabling us to describe the person’s stroke syndrome accurately.
If anyone telephones me about a patient with a lacunar syndrome for example, I immediately know what they are talking about!
This in turn helps me to estimate prognosis and sometimes is a clue to which aetiology and mechanism of stroke are most likely.
The CHADS score is helpful to estimate the risk of stroke in people with atrial fibrillation.
The CHADS score is based on the presence or absence of a history of congestive heart failure, hypertension, age greater than 75 years, diabetes and prior cerebrovascular disease.
Mr. Tanner’s CHADS2 score comes out to 4. It’s important to remember that Mr Tanner still hasn’t had his Echocardiogram done. We need to make sure he doesn’t have valvular disease or other significant structural heart disease.
The CHADS score only helps us to estimate Mr Tanner’s risk of ischaemic stroke. We also need to consider his risk of a haemorrhage if he should commence warfarin therapy.
Unfortunately as risk of stroke increases, the risk of haemorrhage also increases. This was shown in a study authored by Hylek in the 2007 issue of Circulation. If you are interested, the paper is in Volume 115 on page 2689.
There are some data in older people. For example, you can read the BAFTA trial which was published in the Lancet in 2007. Mant is the lead author. The trial is in Volume 370, page 493.
Although it does appear that the benefits of warfarin therapy extend to older people, unfortunately these results may not be generalisable to the very frail patients that you will sometimes look after.
ATRIAL FIBRILLATION can cause strokes by allowing blood to pool and form clots in the poorly contracting atria and especially in the left atrial appendage. These clots sometimes break off and can lodge in the brain. It is likely that Mr Tanner’s TIA was caused by this mechanism.
Operating on low grade stenosis (even if symptomatic) may lead to more complications than future stroke prevention. Have a look at the following link:
mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD001081/frame.html
By the way, thanks for the quick referral. Although carotid endarterectomy is not appropriate in this case, it is important that we see these patients within two weeks of their first symptoms.
Check out the following articles:
Rothwell PM et al. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 2004; 363:915
Fuster V et al. Task force report: ACC/AHA/ESC guidelines for the management of atrial fibrillation. Eur Heart J 2001;22:1852-923
There is a decreasing incidence of stroke (40% over 20 years :OCSP, Oxvasc) related to reduction in traditional vascular risk factors and pharmacotherapy.
However ageing of the population will contribute to doubling of the overall burden of stroke mortality by 2020.
At 6 months after stroke, more than 60% of patients will have died (20%) or be dependent (40%) despite best medical therapy.
Cerebrovascular disease is thought to be the second most common cause of dementia.
Here are some other resources you can refer her to:
Sudlow CLM, Warlow CP, for the International Stroke Incidence Collaboration. Comparable studies of the incidence of stroke and its pathological types: results from an international collaboration. Stroke 1997; 28: 491–99.
Feigin VL, Lawes CMM, Bennett DA, Anderson CA. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol 2003; 2: 43–53.
The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. International Stroke Trial Collaborative Group. Lancet, 1997. 349(9065): p. 1569-81.
Warolow C, Sudlow C. Dennis M, Wardlaw J, Sandercock P. Stroke. Lancet 2003; 363:1211-1224.
TIA’s can predict future stroke risk.
“We do have tools that allow us to determine the risk of future stroke after a transient ischaemic event. The most commonly used tool is the ABCD squared scale which estimates risk based on the patient’s age, blood pressure, clinical features, duration of symptoms and history of diabetes.”
Mr Tanner’s risk of stroke is around 10% at 90 days, and 4% on day 2.
The best management strategy for these patients is still controversial. Often we are concerned that discharge may not be safe if the risk of recurrence is high.
Many centres have focused care for TIA patients on early assessment and intervention to try and reduce the risk of recurrence. For example, you may like to read the results of the EXPRESS study which was published in the Lancet in 2007. You will find the study in Volume 370 on page 1432. Peter Rothwell is the lead author.”
Yes, if you are concerned about aspiration. This should not delay CT.
Yes this is often the most critical early test, to exclude haemorrhage and look for evidence of stroke mimics.
Pleasingly, Mr Tanner’s CT scan is normal.
Yes, this is an important test, and although often requested urgently, is often not available immediately.
Yes, an ECG should be done early to see if the patient is in AF and to look for other evidence of cardiac pathology.
Yes a BSL is especially important to get done urgently, usually by a finger prick. Other tests often ordered include a full blood count and urea and electrolytes. In Mr Tanner’s case, these are both normal.
This is continuous 24 hour ECG monitoring. Yes this is an important test, and although often requested urgently, is often not available immediately.
Yes this is an important test, and although often requested urgently, is often not available immediately.
We know that adherence with prescribed therapies is often suboptimal and thus it is important to check that Mr Tanner was taking his blood pressure medicines as prescribed. Although hypertension is a very strong risk factor for stroke, it’s important to remember that most strokes do occur in people with high normal blood pressure or mild hypertension.
There is conflicting evidence regarding the association between hypercholesterolaemia and the risk of stroke.
There have been epidemiologic studies suggesting that a higher cholesterol level is associated with a higher risk of ischaemic stroke, but a lower risk of haemorrhagic stroke.
There is good evidence that statins reduce the risk of major vascular events for those with stroke who have a total cholesterol of >3.5 and who may or may not have concurrent coronary heart disease.
In secondary prevention aspirin has a well proven role, with a 0.5% reduction in the risk of stroke. The Antithrombotic Trialists’ Collaboration found that the absolute reduction in the risk of having a serious vascular event was 36 per 1000 patients with previous myocardial infarction treated for two years. This study was published in the British Medical Journal in 2002. You can find the article in Volume 324 on page 71.
However aspirin doesn’t stop recurrent strokes. A recent Cochrane review shows that for every 1000 patients treated with aspirin within 48 hours of an acute ischaemic stroke, only 13 patients will avoid death or dependency. This translates to a number needed to treat to benefit of 79.
The benefits of aspirin therapy in primary prevention are not as clear cut. It may be that it is a reasonable to treat men who are at high risk of vascular events, but the balance of risks and benefits is less clear for people at lower risk, and for women.

Time's up
www.strokefoundation.com.au/health-professionals
www.strokecenter.org/prof/index.html
www.sol.co.uk/r/rsmacwalter/sites.html
www.strokecenter.org/trials/scales/modified_rankin.pdf
https://stroke.ahajournals.org/cgi/content/full/26/11/2027

Time's up
Mrs Browning is counselled with regard to the findings of her hearing tests and given strategies that she can implement to assist her hearing in difficult situations. These include:
Mrs Browning is fitted with new glasses and will have bi-yearly vision testing to make sure the macular degeneration does not worsen.
Mrs Browning appears well. She is well presented, and is in high spirits.
Height: 178cms
Weight: 66kg (an increase of 1 kg)
Please move your cursor over Mrs Browning as if you were examining her. You must complete the examination before you go on.
Mrs Browning looks happy and healthy.
Height: 178cms
Weight: 65kg (has remained constant)
Please move your cursor over Mrs Browning as if you were examining her. You must complete the examination before you go on.
General Appearance: Mrs Browning looks well. Her affect is reactive and she doesn’t appear to be distressed or anxious.
Height: 178cms
Weight: 65kg (has remained constant)
Please move your cursor over Mrs Browning as if you were examining her. You must complete the examination before you go on.
Insomnia can be a symptom of an underlying medical conditions including asthma, allergy, arthritis, heart disease, hyperthyroidism, or Parkinson’s disease. It can also occur as a result of pain, jet lag, caffeine, trauma, medications, anxiety, depression, or environmental factors such as noise or heat. Take a relevant history and conduct the necessary assessments to determine the most likely cause of Mrs Browning’s insomnia.
In order to take a sleep history, you will need to ask Mrs Browning a series of questions. Please click on the questions below to obtain Mrs Browning’s answer.
Well, I suppose it has been ongoing for the last 5 or 6 months.
Very gradual, although it has gotten worse over the last few months.
No. I’m usually quite sleepy in the evenings, so getting to sleep isn’t a problem.
Yes, I do tend to wake up at least a few times during the night. Sometimes, I can’t get back to sleep for a long time and have to get up and read a book for a while.
I generally wake up very early these days, around quarter to five or 5am. I often can’t get back to sleep, so I get up and make myself a cup of tea and watch the early news until Denny wakes up.
No, nothing like that.
No.
No, not at all. I live on a very quiet street.
Excessive noise can disrupt sleep.
I’ve tried natural remedies, such as valerian and a herbal flowers sleep remedy. I’ve also tried having a warm bath before bedtime, but nothing seems to help.
Oh, it’s been good. I’m almost always in a good mood. I’ve a lot to be thankful for. I’m looking forward to our retirement years.
Sometimes insomnia can indicate a mood disorder, such as depression or even mania.
No, I’m pretty relaxed and still enjoy my life. I’m looking forward to retirement, although I do sometimes worry about the future.
Anxiety and stress (including the stress of retirement or bereavement) can cause insomnia.
Just a little bit of pain from my arthritis.
Oh, only about a 1 or 2. It’s not bad at all really and it usually goes away if I take a couple of paracetamol tablets.
Pain, especially pain from arthritis or lower back pain, are often linked with insomnia.
No, I’m as fit as a mallee bull.
No, never.
Angina or orthopnoea (breathlessness on lying down), could indicate heart disease as a potential cause of insomnia.
No, this has never been an on-going problem for me. I only had it when I had that chest infection a couple of years ago.
Wheezing or a nocturnal cough may indicate asthma as a possible cause of insomnia.
No. Occasionally I might have to get up once, but I try not to drink too much fluid later in the evening so I don’t get a full bladder during the night.
Insomnia is sometimes caused by nocturia, and is important to take a careful history for urinary symptoms.
No
Polydipsia is sometimes associated with diabetes and can contribute to insomnia.
No, I’ve always liked the warmer weather.
Intolerance to heat can be a sign of hyperthyroidism.
No
Well, I take paracetamol occasionally if I have pain from my arthritis or a headache. I also regularly take calcium, vitamin B12, ginko biloba, flaxseed oil and olive leaf extract.
It is important to make sure Mrs Browning has not suddenly changed, stopped or commenced any medications, including over the counter or herbal. See below is a table of common substances and their effects on the body.
I have a cup of tea if I wake up early in the morning and can’t sleep. Then I’ll have a coffee with Denny when he wakes up, and another cup of tea mid-afternoon. I drink herbal tea at the other times.
Caffeine is a stimulant and can cause insomnia.
I occasionally have a nip of brandy or Irish Cream liquor after dinner. Probably only once or twice a week.
Mrs Browning appears to consume a total of 2-3 units of alcohol a week. This is within the current guidelines for safe consumption of alcohol. For further information see the link below.

Time's up
https://www.ehealthmd.com/library/insomnia/INS_causes.html
https://www.helpguide.org/life/sleep_aging.htm
https://www.uptodate.com/patients/content/topic.do?topicKey=~ljjjZJvihvvMX6
https://www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/ateaf/1979359?open
https://nei.nih.gov/health/cataract/cataract_facts
https://www.mayoclinic.org/news2007-mchi/4220.html
https://www.nlm.nih.gov/medlineplus/ency/article/001045.htm

Time's up
The Home and Community Care (HACC) Program provides basic support and maintenance services to frail aged people, younger people with disabilities and their carer to assist them to continue living independently at home. The types of support include:
Berg Balance Scale
The physiotherapy consult finds Mr Doherty’s Berg balance scale is 46/56. He had difficulty turning to look behind, reaching, retrieving an object from the floor and balancing on one foot. He had a positive Rhomberg test, with persistant sway while standing with eyes closed.
The physiotherapist prescribed specific balance exercises, which can be performed as a home program.
Gait Assessment
Mr Doherty had no trouble transferring or turning in the timed up and go test, completing the assessment in 11.3 seconds. His gait velocity and character were normal. Mr Doherty has some problems with balance, but no significant falls risk as a result of this.
However, in conjunction with his poor eyesight, his risk of having a fall is increased.
Berg Balance Scale
The assessment finds Mrs Doherty’s Berg balance scale is 32/56. She has difficulty transferring, turning, reaching and balancing on one foot. She also had a positive Rhomberg test, with significant irregular sway while standing with eyes closed.
The physiotherapist prescribed specific mobility exercises (including stretches in prone lying) and specific strengthening exercises for the leg extensors, which can be performed as a home program.
It is important that Mrs Doherty maintain these exercises, in order to maintain muscle strength and joint range of movement and to improve her balance.
Gait Assessment
Mrs Doherty has a mildly hemiparetic gait related to her residual right sided weakness. There is impaired timing and intensity of muscle action in the right leg, which affects gait velocity and character. She also has mild upper kyphosis. She had trouble with the timed up and go test due to difficulty transferring and gait impairment. Her time for the assessment was 26.7 seconds.
Given this, Mrs Doherty has significant falls risk.
Mrs Doherty gave up her driver’s license 7 months ago. With increasing shortness of breath, tiredness, chest pains and reflux, she has become increasingly unable to shop, prepare food, clean the house, do laundry or adequately administer her medications. She does a good job of managing the household finances
Mrs Doherty is continent and is able to dress, feed and go to the toilet herself. She is having some trouble showering and using her upper extremities due to extreme shortness of breath and fatigue. As a result her personal hygiene and presentation have been affected
Geriatric Assessment Tools
On their own, screening tests are not able to diagnose dementia as they test limited domains of cognition. They can be useful in identifying someone needing further investigation and are also useful if done serially to map any change in cognition over time.
The ideal screening test would be both sensitive (high rate of true positive) and specific (high rate of true negatives results). However this is not as straight forward as it sounds, because positive predictive value of tests is also influenced by the prevalence of the disease condition! Keep in mind too that “cut offs” are based on population norms or empiric studies and thus can not be considered in isolation.
Please click on the tabs below to reveal more information about each of the commonly used screening tools.
The Mini Mental State Examination
The MMSE is the most common test for screening for cognitive impairment. It tests multiple cognitive domains including orientation in time and place, attention, calculation, short term memory, language and copying. It helps to quantify the patient’s degree of impairment, and may be followed over time to track the progression of impairment. It is however, poor at detecting very mild dementia and does not test frontal/executive function and visuospatial function well, making it less valuable in non-Alzheimer’s type dementias. A score of 24/30 or below is suggestive of cognitive impairment, although a ‘normal’ MMSE does not rule out the possibility of cognitive impairment, especially in younger or well-educated patients. This test usually takes around 10 minutes to complete.
The Clock Drawing Test
This is a screen for visuospatial, constructional praxis and frontal executive impairment that takes 1 or 2 minutes to complete. It is a simple bedside test that is independent of bias due to intellect, language or cultural factors. The clock drawing test does not detect early cognitive changes or discriminate between types of dementia raising questions about its suitability to be used in isolation.
There are a number of alternative ways of administering and scoring the CDT, such as those described by, Shulman (1993), Sunderland (1989) and Wolf-Klein (1989). Of these, the Shulman method has been found to be the most sensitive and specific screening test for mild-moderate dementia when used in conjunction with MMSE.
In the Shulman method, subjects are asked to add the numbers of a clock-face on to a pre-drawn circle and to mark in the hands to resemble a specified time. Results are scored as follows:
It is a good idea to read the following article to familiarise yourself with each the commonly used CDT methods, as they are frequently used by doctors, allied health professionals and ACAT nurses.
Brodarty H and Moore C. 1997. The Clock Drawing Test For Dementia Of The Alzheimer’s Type: A Comparison Of Three Scoring Methods In A Memory Disorders Clinic. International Journal of Geriatric Psychiatry, 12: 619-627.
GPCOG
This brief validated screen (specifically for Primary Care) incorporates the Clock Drawing task. The test is available online.
Geriatric Depression Scale
The Geriatric Depression Scale is commonly used to screen mood disorder which may impact on performance of other cognitive assessments. A score of 5 or more is suggestive of an underlying mood disorder and further clinical assessment is recommended.
There has been some concern about its accuracy in detecting minor depression. It is suitable for use with people with a Mini-Mental Status score of more than 14. It takes 5-10 minutes to complete.
The Geriatric Depression Scale is available in many languages.
Most screening tests for dementia involve a brief list of questions to directly assess cognitive functioning, such as the MMSE. A disadvantage of such tests is that they are affected by the person’s level of education, familiarity with the dominant language and culture in their country, and level of intelligence before the onset of dementia. Because of this, cognitive screening tests can falsely indicate dementia in people with lower education, culturally and linguistically diverse backgrounds, and lower intelligence. The IQCODE attempts to overcome this problem by assessing change from earlier in life, rather than the person’s current level of functioning. It does this by making use of the informant’s knowledge of both the person’s earlier and current cognitive functioning. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) is a questionnaire that can be filled out by a relative or carer (the informant) of an older person to determine whether that person has declined in cognitive functioning. The IQCODE is often used as a screening test for dementia.
IQCODE is especially useful in cases where, for different reasons, a meaningful formal cognitive assessment cannot be performed. It also gives the relative an opportunity to say what they feel. IQCODE has been found to have similar specificity and sensitivity to the MMSE.
To score the IQCODE, add up the score for each question and divide by the number of questions (for the short IQCODE, divide by 16). A cut-off point of 3.31/3.38 achieves a balance of sensitivity and specificity.
Jorm, A. F. (1994). A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): Development and cross-validation. Psychological Medicine, 24, 145-153
The Frontal Assessment Battery is a brief tool that can be used at the bedside or in a clinic setting to assist in discriminating between dementias with a frontal dysexecutive phenotype and Dementia of Alzheimer’s Type (DAT). The FAB has validity in distinguishing Fronto-temporal type dementia from DAT in mildly demented patients (MMSE > 24). Total score is from a maximum of 18, higher scores indicating better performance.
Slachevsky: Frontal Assessment Battery and Differential Diagnosis of Frontotemporal Dementia and Alzheimer Disease. Arch Neurol. 2004;61:1104-1107
Alzheimer’s Disease Assessment Scale – Cognitive (ADAS-Cog)
The Alzheimer’s Disease Assessment Scale (ADAS) of which one section is the ADAS Cog, evaluates cognitive functions affected in Alzheimer’s disease including memory, language and praxis. This 11-part test is more thorough than the MMSE and can be used for people with mild symptoms. It is a commonly used for brief examination of memory and language skills and is often used as a measure in clinical drug trials. It takes around 30 minutes and can be conducted by several members from the multidisciplinary team (such as a doctor, nurse, OT or psychologist)
AMTS
This brief 10 item screen takes about 3 minutes to administer, It includes components requiring intact short and long term memory attention and orientation.
One point is allocated for each correct response. A score of <8/10 is suggestive of significant cognitive deficit, although further and more formal tests are necessary to confirm the diagnosis. Results areaffected by language and cultural background. Its advantage is its brevity.
Hodkinson, HM (1972). "Evaluation of a mental test score for assessment of mental impairment in the elderly.".Age and Ageing 1 (4): 233-8. https://ageing.oxfordjournals.org/cgi/reprint/1/4/233.
RUDAS
Australia is culturally diverse, with many people who have non-English speaking backgrounds (NESB). Unfortunately this can make the MMSE difficult to use as many of the concepts do not translate easily. A new tool was developed and validated in the multicultural population of South West Sydney: the Rowland Universal Dementia Assessment Scale – (RUDAS). The score is affected by age but it is not affected by educational level or preferred language. (Storey, Rowland, Conforti, and Dickson 2006). This test is most applicable to people with limited ability to speak or understand spoken English and, unlike the other tests, it remains reliable when administered through an interpreter.
This tool is commonly used by allied health staff and ACAT nurses.

Time's up

Time's up

Time's up

Time's up
Click on the following blood tests to see the result and the rationale for ordering each test.
White cell count 7.2x109/L (normal range 4.0-11.0x109/L for adult males)
Neutrophil count 4.8x109/L (normal range 2.0-7.5x109/L)
Haemoglobin 142 g/l (normal range 135-180 g/l for adult males)
Mean cell volume 92 fl (normal range 80-100 fl)
Platelets 320x109/L (normal range 150-400x109/L)
Infection can cause delirium, but Dr Zheng’s results are normal.
Sodium 141 mmol/L (normal range 134-146 mmol/L)
Potassium 3.4 mmol/L (normal range 3.4-5.0 mmol/L)
Urea 6.9 mmol/L (normal range 3.0-8.0 mmol/L)
Creatinine 78 µmol/L (normal range 60-120 µmol/L for adult males)
Calcium 2.5 mmol/L (normal range 2.15-2.60 mmol/L)
Electrolyte disturbance (eg hyponataemia) can exacerbate confusion, but Dr Zheng’s results are within normal range.
Glucose: negative
Bilirubin: negative
Protein: 5mg/dL
RBC’s: <4 RBC/high power field (normal)
WBC’s: negative
Dipstick test: negative for bacteria
To assess possibility of UTI (may cause delirium) renal disease or other diseases. Dr Zheng’s results are normal, suggesting underlying renal or urinary tract problems is less likely.
ESR 22 mm/hr (normal range 1-30 mm/hr for adult males)
To rule out possible delirium. Dr Zheng’s result is within normal range.
Dr Zheng currently has only mild dementia and can predominantly perform all Activities of Daily Living (ADL’s) independently. At present, the Zheng’s are confident that they can manage all of his care needs without further assistance.
I have let Mrs Zheng and her daughter know that I will remain in regular contact to provide carer support and have encouraged them to contact me if they have any difficulties or would like to enlist care assistance as Dr Zheng’s dementia progresses. As the Zheng’s live in the country, there is no local carer support group, but I will arrange for them to participate by video-conferencing. Facilities are available for this service through the regional hospital telehealth centre. I have also discussed grieving and loss with the Zheng family and provided information about support services that are available. I will regularly follow-up with the Zheng family to assess their needs. I have also informed their GP of the situation and suggested he be aware of the potential for depression and/or carer fatigue in Mrs Zheng’s case.
I have given The Zheng’s further written information on dementia and its course and concluded that they do not require any assistance from Home and Community Care (HACC) at this stage. This will be reviewed at yearly intervals unless otherwise requested. We have discussed local services available through the Aged Care Assessment Team (ACAT) and Home and Community Care (HACC) and the Zheng’s have been provided with additional information on these services and how to access them.
Many people with dementia are concerned that their disease may have been inherited and that they may pass it on to their children. Family members of people with dementia are sometimes concerned that they might be more likely to develop dementia themselves. Genes do play some role in the development of dementia, but their specific effects vary considerably.A number of genes have been implicated in the onset of DAT. Studies of familial early-onset DAT, which accounts for less than 1% of all DAT cases, have identified mutations in three genes that account for up to 50% of such cases.If a parent has dementia, their illness is most likely due to a combination of many genes working together with lifestyle factors. It is unlikely that the child of this parent would inherit all the disease susceptibility genes, although the risk of disease is slightly increased compared to someone without a relative with dementia.The following resources outline the present state of knowledge about the inherited risk of dementia:
www.alzheimers.org.uk/factsheet/405
Information may need to be added later
Written information about dementia can be helpful to take away and provides a helpful reference. Alzheimer’s Australia has information specifically for people with dementia.
Contact the National Dementia Helpline on 1800 100 500
What information to share
As a general guide a number of things need to be explained. These include:
Informing a person that they have dementia is a serious matter, which needs to be handled with great sensitivity, calmness and dignity. It can be a very stressful time for everyone. Don’t forget to look after carers, and yourself! Alzheimer’s Australia offers confidential counselling and support for families, carers and people with dementia.
Contact the National Dementia Helpline on 1800 100 500.
Based on:
The right to know? Sharing the diagnosis of dementia, by K Fearnley and D Weeks, and Communicating the diagnosis, Alzheimer’s Society, Canada
Iliffe S et al. 2009. Primary care and dementia: 1. diagnosis, screeningand disclosure. International Journal of Geriatric Psychiatry; 24: 895–901.
Blood tests are routinely used in dementia diagnosis mainly to exclude potentially reversible causes of cognitive decline. These include active infection (white cell count), hyperthyroidism, hypothyroidism, B12 deficiency, renal and liver failure and to record folate, glucose, calcium and cholesterol levels.
Click on the tabs below to view the results.
WBC 7.6x109/L (normal range 4.0-11.0x109/L)
Neutrophils 4.1x109/L (normal range 2.0-7.5x109/L)
Hb 139 g/l (normal range 135-180 g/l for adult males)
MCV 89 fl (normal range 80-100 fl)
Platelets 313x109/L (normal range 150-400x109/L)
Infection or blood dyscrasia can be a possible cause of dementia-like symptoms, but Dr Zheng’s results are normal.
546 pmol/L (normal range 120-680 pmol/L)
A vitamin-B12 level should be obtained to evaluate for a reversible cause of dementia-like symptoms. Dr Zheng’s levels are within normal limits, so this is not the cause of his memory problems.
Creatinine 97 µmol/L (normal range 60-120 µmol/L for adult males)
Urea 8 mmol/L (normal range 3.0-8.0 mmol/L)
Renal function is assessed to rule out metabolic disturbance or kidney dysfunction that can cause dementia-like symptoms. Dr Zheng’s tests are normal.
Sodium 142 mmol/L (normal range 134-146 mmol/L)
Potassium 3.7 mmol/L (normal range 3.4-5.0 mmol/L)
Calcium 2.18 mmol/L (normal range 2.15-2.60 mmol/L)
Electrolytes disturbance (eg hyponataemia) is a common cause of confusion, but not in Dr Zheng’s case – his results are within normal range.
AST 26 U/L (normal range <45 U/L for adult males)
ALT 17 U/L (normal range <40 U/L for adult males)
Bilirubin 16 µmol/L (normal range <20 µmol/L)
ALP 88 U/L (normal range 35-135 U/L)
GGT 57 U/L (normal range <60 U/L for adult males)
Albumin 39 g/L (normal range 35-50 g/L)
Liver dysfunction is a possible cause of dementia-like symptoms, but once again, Dr Zheng’s results are normal.
Glucose 5.2 mmol/L (normal range 3.0-5.4 mmol/L)
Hypoglycaemia can cloud cognitive function and therefore simulate dementia. Results show this is not the case for Dr Zheng.
ESR 20 mm/hr (normal range 1-30 mm/hr for adult males)
To rule out potential reversible causes of dementia-like symptoms, by indirectly measuring how much inflammation is in the body. Dr Zheng’s result is within normal range.
TSH 1.6 mU/L (normal range 0.40-4.0 mU/L)
Free T4 12.4 pmol/L (normal range 9-19 pmol/L)
Metabolic disturbances are a possible cause of dementia-like symptoms, but Dr Zheng’s results are normal.
Not ordered (normal range <6.1 ug/L for men over the age of 70)
Not required in the investigation for dementia – but reasonable test to consider if Dr Zheng has prostatism.
Cholesterol 4.6 mmol/L (normal range <5.5 mmol/L)
HDL 1.2 mmol/L (normal range >1.0 mmol/L)
LDL 1.7 mmol/L (normal range <3.0 mmol/L)
Triglycerides 1.9 mmol/L (normal range <2.0 mmol/L)
May be considered to assess Dr Zheng’s vascular risk.
Not ordered
The UA is not necessary for the diagnosis of dementia – but may be useful if UTI is suspected.
Please move your cursor over Dr Zheng as if you were examining him. You must complete the examination before you go on.
No tremor is observed. He is well groomed and does not appear anxious. He has normal attention and affect.
Height: 160cms
Weight: 70kgs
Temperature: 37.1
Please move your cursor over Mr Thomas as if you were examining him. You must complete the examination before you go on.
Just the aspirin if I get headache that will not go away.
No, nothing
Yes, I take a chinese herb as blood tonic. It help to balance the Ying Yang energies in the body and keep all organs working well. I also have acupuncture and most times this helps with my headaches.
My wife will say only to housework!
Yes, a few times in China. It was a long time ago, when I was younger. I can't remember all of them. I know one time it was for gastroenteritis
Headache sometimes,but that's about it these days.
Past medical history may be relevant to cause, presentation and treatment of cognitive impairment.
I had my appendix out when I lived in China. It was a while ago. I also had a mole on back remove not so long ago. I can't remember exactly when.
No, just the headaches every so often.
No.
No, nothing like that.
These question can help to rule out other potential causes of cognitive decline such as those related to infection or inflammation.
My wife think I need to see a doctor because I can't remember some things. She is nagging me for years! And my doctor say I should come to Perth for an assessment. That's why I am here.
No - not forgetful. My wife think so, she is always telling me that I forget things. I think she is over reacting. Somethings might slip my memory from time to time, but that is just part of getting older.
Well, once or twice I might forget meeting, or appointment - but that is just because so busy - helping May at the restaurant
Which of the following medications can potentially cause cognitive problems?
Click each to find out.
Yes – some antidiarrhoels are anticholinergics
Not usually – though hypo and hyper glycaemia are occasional causes of confusion
Yes – sedation is a common side effect of anti-epileptics
Not usually – although some people find antiinflammatories cause a “fuzzy head”
Yes – if anticholinergic side effects
Not usually
Yes – lithium is commonly sedating
Yes – benzodiazepines are notorious for causing “hang over” effects
Not usually – but think of intracranial bleeding if any patient on warfarin becomes acutely confused.
Yes – these “dirty drugs” have anticholinergic toxicity
Yes – “chemo brain” is well described

Time's up
The Dementia Lecture was supported by the WA Dementia Training Study Centre.
Lecture by Dr Kenneth Rockwood
Bridges-Webb C and Wolk J. Care of Patients with Dementia in General Practice: Guidelines. Royal Australian College of General Practitioners; Sydney, 2003
Dysch L. 2003. Using the Clock Drawing Task in primary care. Geriatric Medicine September 2003. Eastly R., Assessment of Dementia, in Dementia. Eds Burns, O’Brien and Ames. London: Hodder Arnold, 2005.
Feinberg T., and Goodman B. 1984. Affective illness, dementia and pseudodementia. Journal of Clinical Psychiatry. 45; 99-103.
Feldman H et al. 2008. Diagnosis and treatment of dementia: 2. Diagnosis. Journal of the Canadian Medical Association. 178; 7: 825-836
Hecker J., Dementia and Alzheimer’s Disease, in A Practical Guide to Geriatric Medicine. Ed Ratnaike R. McGraw-Hill Professional Publishing, 2002
Hogan D et al. 2008. Diagnosis and Treatment of Dementia: 4. Approach to management of mild to moderate dementia. Journal of the Canadian Medical Association. 179: 8: 787-793
Hogan D et al. 2008. Diagnosis and Treatment of Dementia: 5. Nonpharmacologic and pharmacologic therapy for mild to moderate dementia. Journal of the Canadian Medical Association. 179: 10: 1019-1026
Juby A, Tench S, Baker V. The value of clock drawing in identifying executive cognitive dysfunction in people with a normal Mini-Mental State Examination score. Canadian Medical Association Journal 2002; 167(8): 859Ð64
Suresh et al. 2008. 10-Minute Consultation: Memory problems in an older person. BMJ. 337: a1170
Watson JD. 2001. Disorders of Memory and Intellect. Medical Journal of Australia. 175; 433-437.
https://www.dementiacareaustralia.com/index.php/library/what-is-dementia.html
https://www.agedcareaustralia.gov.au/internet/agedcare/publishing.nsf/Content/What%20is%20dementia
NICE Clinical Guideline 42; Dementia – Supporting people with dementia and their carers in health and social care. Developed by the National Collaborating Centre for Mental Health, UK. www.nice.org.uk
Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98.

Time's up
Other medication strategies may include stimulants, mood-stabilising medications, anti-anxiety medications or antipsychotic medications. In some cases the combination of two or more antidepressants or other medications may be used to augment the action of antidepressants.
Tricyclic antidepressants (TCA’s) maybe considered if first line treatments are unsuccessful. These are as effective in treating depression but tend to be associated with more side effects than SSRIs.
Tricyclic antidepressants (TCAs) have been in use for more than 40 years. Despite this, we do not know exactly how they work. However, they do affect the chemicals noradrenaline (also known as norepinephrine) and serotonin. These chemicals are neurotransmitters and they are made by the cells in the brain. Neuorotransmitters are the means by which the brain cells connect and communicate with each other. The tricyclic antidepressants increase the amount of noradrenaline and serotonin in the brain. They also effect other neurotransmitters which cause some side effects (such as dry mouth). Over many years of study and use tricyclics have been shown to improve symptoms of depression and anxiety. They also reduce obsessions and compulsions in obsessive-compulsive disorders (OCD).
Common side effects include:
Another common first line drug option for the treatment of depression are Tetracyclic Antidepressants, such as Mianserin. These drugs prevent neurotransmitters from interacting with nerve cell receptors. This indirectly increases the levels of neurotransmitters and serotonin in the brain.
Common side effects may include:
Other common first line drug options include SNRI’s (serotonin and norepinephrine reuptake inhibitors) like venlafaxine.
Serotonin and noradrenaline (also called norepinephrine) are neurotransmitters made by the cells in the brain. Neurotransmitters are chemicals used by brain cells to connect and communicate with each other. SNRI antidepressants slow the rate that the brain breaks down serotonin and noradrenaline. This leads to an increase in serotonin and noradrenaline activity in the brain. (Mirtazapine has a similar effect by a slightly different mechanism.) This has been shown to improve symptoms of depression and anxiety. It also reduces obsessions and compulsions in obsessive-compulsive disorders (OCD).
Common side effects include:
The effect on weight is unclear, however appetite reduction and weight loss most likely with Venlafaxine (Efexor) and Nefazadone (Serzone)
Weight gain most likely with Mirtazapine (Remeron/Avanza)
The effect on sleep is unpredictable, however broken sleep is common with some of the SNRI medications (Venlafaxine, Efexor)
Other SNRIs may cause sleepiness (Mirtazapine, Remeron/Avanza)
SSRI’s (selective serotonin reuptake inhibitors) are usually the first choice of drugs used to treat depression. This family of anti-depressants is often effective and tends to have fewer side-effects. Common SSRI’s include include sertraline, citalopram and fluoxetine.
Serotonin is a neurotransmitter made by the cells in the brain. Neurotransmitters are chemicals used by brain cells to connect and communicate with each other. SSRI antidepressants slow the rate that the brain breaks down serotonin. This in turn causes an increase in serotonin activity in the brain. This has been shown to improve symptoms of depression.
Common side effects include:
The effect on weight is unclear, however appetite reduction and weight loss most likely with fluoxetine and weight gain is possible with some other SSRIs.
The effect on sleep is unpredictable, however broken sleep is common with some of the SSRI medications (Fluoxetine, Prozac/Lovan), while others may cause sleepiness (Fluvoxamine, Luvox).
SSRIs may also cause intensified dreaming.
The DSM-IV criteria for a diagnosis of depression are:
Five or more of the following symptoms have been present most of the time for at least 2 weeks; at least one symptom is either a depressed mood or anhedonia:
1. Depressed mood
2. Anhedonia
3. Significant weight change or change in appetite
4. Insomnia or hypersomnia
5. Psychomotor agitation or retardation
6. Fatigue or loss of energy
7. Feelings of worthlessness or excessive guilt
8. Decreased ability to concentrate or indecisiveness
9. Thoughts of death or suicidal ideation
·Symptoms do not meet the criteria for a mixed episode
·Symptoms cause significant distress or impairment in functioning
·Symptoms are not due to substance abuse, medication, or a medical condition
·Symptoms are not better accounted for by bereavement.

Time's up

Time's up
Managing the pain and stiffness of Mrs Scott’s arthritis may well improve her experience of functional incontinence by helping her to move around more easily.
The physiotherapy assessment reveals that Mrs Scott has significant joint changes indicative of osteoarthritis particularly affecting her hands, shoulders, ankles and knees. She has reduced grip strength in both hands and hip and knee extensor strength is diminished (unable to rise from a standard chair without using her arms to push off). Joint range is restricted in shoulders, knees, ankles, cervical and lumbar spine.
Mrs Scott is encouraged to maintain her participation in physical activity, particularly water based activity that facilitates a greater joint range of movement. Light weight bearing activity will prevent further muscle loss and increase bone strength. Mrs Scott is slightly overweight and may benefit in speaking with a dietitian. A reduction in body mass may alleviate strain on her joints and therefore lessen the symptoms of arthritis.
She will continue to take paracetamol, as needed, for pain management.
A home OT assessment is performed to address Mrs Scott’s problem with falling whilst trying to make it to the toilet. She reports that she most often falls at night when she wakes up and has to get to the toilet in a hurry. On assessment the OT notices that there are no bedside lamps that can easily be switched on in the night and neither is there low level hallway lighting. The OT therefore recommends touch lamps that can easily be accessed and operated before getting out of bed so that Mrs Scott can easily see where she is going. Night lights should also be installed in the hallway.
The lamp shades in the living areas provide adequate light, with open shades and 80 watt globes and all apartments in the retirement village are fitted with motion sensor outdoor lights that turn on automatically so that the entryway is well lit when Mr and Mrs Scott return home in the evening.
There were a couple of mats in the hallway and lounge room that were considered tripping hazards and it was recommended that these be removed or taped down. Non-slip surfaces were laid in the toilet, bathroom, laundry and kitchen areas and recommendations were made for grab bars in the bathroom and toilet frame.
The Scott’s live in a single story ground floor apartment with no steps or stairs, so these are not an issue for falls risk.
It is likely that Mrs Scott’s orthostatic hypotension with a 35mmHg Systolic drop is a contributory factor in her night time falls. It is likely that this will improve as Mrs Scott adjusts and improves her fluid intake, but she is advised to sit on the side of the bed for a few minutes if possible to allow her blood pressure to accommodate and therefore avoid any dizziness when standing. She may also benefit from using a walking frame at night when rising from bed to use the toilet.
They are given information about personal alarms that Mrs Scott can keep on her at all times. This way, she can raise the alert if she ever has a fall and is unable to reach a telephone to call for help in the event that Mr Scott might not be at home. The alarm can also be used for any other medical or personal emergency and helps provide peace of mind.
Mrs Scott looks well. She is reactive but has restricted mobility.
Height: 164cms
Weight: 76kg (which has remained constant)
Please move your cursor over Mrs Scott as if you were examining her. You must complete the examination before you go on.
Continue to interview Mrs Scott by clicking on the questions below…
I’d say about 4 times, although I never used to fall as often as I do these days. Now that Robert is sleeping better, I don’t wake him up to help me if I’ve fallen.
No, nothing at all.
Some medications, particularly sedatives, antidepressants, heart medications, blood pressure medications, antihistamines and cold tablets, can precipitate incontinence.
Yes, I take glucosamine for my arthritis and psyllium for bowel health and a general health tonic.
High doses of vitamin C and vitamin B12 can cause polyuria.
I haven’t been swimming or water aerobics as often, as I can’t use the pads in the pool, but I have still been doing my weights and yoga because of my family history of osteoporosis.
No, I just deal with it and get on with things. It’s just a part of life. I am a bit worried about having an accident in public though. That’s part of the reason why I don’t have too many drinks during the day. I also wear a pad everyday, just in case. I suppose it does get me down from time to time because it makes me realise I’m getting old. And of course it is embarrassing to lose control of your bladder. But I try not to let it stop me from doing things.
I have one cup of tea after each meal.
Caffeine is a diuretic that can cause polyuria.
Only enough to take my tablets. I don’t drink too much so that I don’t urinate as much.
Yes, I don’t have any problem there.
No, nothing that I’ve noticed.
Mrs Scott, these symptoms you are experiencing with your bladder, they are not a normal part of getting older or due to having had children. It is very possible that we can identify what is causing the problem and successfully treat it.
Yes, I guess so. It would be a relief not to wear those pads and not to have to worry about having an accident when I’m out. And it would be great to go to the pool again!
Your role is to take a relevant history to enquire about Mrs Scott’s continence problems and conduct the necessary assessments to determine the most likely cause.
Please click on the questions below to obtain Mrs Scott’s answer.
Oh about 3 or 4 years now. I didn’t think to mention it sooner because it’s been going on for so long, I guess I’m used to it. I’ve learned to live with it and tend to catch up on my sleep with a nap after lunch.
Well, I suppose about 5 times on average.
I wouldn’t say no to a better night’s sleep, that’s for sure. But I’ve had 3 children and I am 75, so what else can I expect? I’ve just accepted it.
Yes, I suppose I do go quite frequently, so I try not to drink too much fluid during the day.
Yes, the feeling that I need to urinate does come on quite suddenly, sometimes with no warning at all and then I can’t seem to hold on. Unless there is a toilet nearby, I sometimes don’t make it in time.
Yes, recently I have felt a deep pain and a dragging feeling after I finishing urinating. Sometimes there is blood on the toilet paper too. I’ve had quite a few urinary tract infections over the years.
Yes, that’s no problem.
Well, I’m often rushing to get there, but I can’t move fast on account of my arthritis. I guess that’s part of the reason why I sometimes don’t get there in time.
Yes, it’s just getting there on time that’s the problem. The flow seems pretty normal, compared to what it has always has been. Except for the pain towards the end, that can be excruciating.
Yes, I do sometimes lose a bit of urine in those circumstances.
Yes, yes I have. I’ve fallen a few times at night when I get up and have to rush to the toilet.
Continue to interview Mr Scott by clicking on the questions below.
No, those things don’t seem to make any difference.
No, nothing at all.
Some medications, particularly sedatives, antidepressants, heart medications, blood pressure medications, antihistamines and cold tablets, can precipitate incontinence.
No, nothing else.
High doses of vitamin C and vitamin B12 can cause polyuria.
Yes, I’ve been pretty down. I just feel so useless, wetting my pants all the time. I’m so embarrassed that I can’t talk to Veronica about it and I guess that might be affecting our relationship. Also, I don’t want to burden her with any more work, so I try to clean up after myself and rinse out my clothes and underclothes, hoping she won’t notice. I don’t want to go anywhere or play any sports because I’m afraid what happened at choir practice will happen again. I suppose not sleeping well is not helping either.
I suppose I’d have about 3 or 4 cups a day. I always have coffee in the morning and then I usually drink tea for the rest of the day.
Caffeine is a diuretic that can cause polyuria.
Only one or two beers or wines on the weekend and a couple of diet cokes a day.
Probably only two, when I take my tablets.
Yes, regular as clockwork. Right after my morning coffee. I take the newspaper in with me!
No, nothing that I’ve noticed.
I’d just love a good night’s sleep and to be able to sing and play sport and generally just be socially active without the fear that I might wet myself.
Your role is to take a relevant history to enquire about Mr Scott’s continence problems and conduct the necessary assessments to determine the most likely cause.
Please click on the questions below to obtain Mr Scott’s answer.
Well, to tell you the truth, I’m really tired and worn out.
No, not at all well over the last few months. My bladder has me up at least 3 or 4 times a night to go to the loo. And Sheila is up often too, so we don’t get more than a couple of hours sleep in a night.
Well, it’s a little embarrassing to talk about, umm I ah, have trouble starting to urinate, even though I often dribble a bit into my underpants on the way there.
Pretty weak, it just kind of trickles out. But my bladder still feels full, so I just keep standing there hoping something more will happen. Then an hour later I’m right back there again.
Yes, I’m embarrassed to say that that has happened once. It was at choir practice. I needed to go to the loo, but it was busy. I was waiting but I couldn’t hold on and I went ahead and wet my pants.
Yes, I’m embarrassed about the dribbling and needing to go so often, but losing control of my bladder, that was the worst. I couldn’t hide it from anyone and I was just humiliated.
No.
No, I don’t get a sudden urge. It’s just that I often feel like I’ve got a full bladder, so I need to go alot. If I wait too long I can’t hold on, so sometimes I don’t make it to the toilet on time.
Yes, that’s no problem.
Bent S et al. (2006) Saw palmetto for benign prostatic hypertrophy, New England Journal of Medicine. 2006;354:557-566 URL: https://content.nejm.org/https://content.nejm.o/
Continence Module Test Answers
CONTINENCE – Notes modified from Dr Kate Scott
URINARY INCONTINENCE – Tutorial by M Donaldson
Constipation Teaching for Interns – Dr Massarotto
“First Steps in Management of Urinary Incontinence in Community Dwelling Older People – A clinical practice guideline 2005”
“Second Steps in Management of Urinary Incontinence in Community Dwelling Older People – A clinical practice guideline for secondary level clinicians”
Developed by Queensland Health and downloadable from https://www.health.qld.gov.au/mass/resourcescont.asp

Time's up

Time's up
Patient answered greeting when approached. He is sitting in a chair with no evidence of agitation or distress. Mr Thomas is now eating a full diet, opens bowels daily and urine output is in keeping with fluid intake. His mouth is moist and mucosa intact. The IV access is removed.
Height: 168cms
Weight: 75kgs
Temperature: 36.7
Respirations: 18 even
Cognitive Testing
MMSE – 25/30 – may indicate resolution of delirium
KICA – 35/39 –Improvement in KICA score supports diagnosis of delirium.
Mrs Thomas does not think Mr Thomas is quite back to baseline, but is improving day by day.

Time's up
Mr Thomas is sweating and looks short of breath. His legs are constantly moving and he appears confused and agitated. His skin is moist and tribal scarring is noted on left and right upper arms, midline of chest and left and right thighs. His eyes are wandering and he appears to have trouble maintaining attention, although this does fluctuate. Admission staff report that his speech was slow and at times, incoherent. Mr Thomas also exhibited impaired orientation. His wife reports that he had trouble sleeping last night.
Height: 168cms
Weight: 75kgs
Temperature: 36.7
Respirations: 28 shallow
Please move your cursor over Mr Thomas as if you were examining him. You must complete the examination before you go on.
Continue to interview Mrs Thomas by clicking on the questions below…
Only those pills when he has pain – you know – paracetamol.
Medication side effects and interactions are one of the most common causes of delirium.
Yes
Medication side effects and interactions are one of the most common causes of delirium.
No
Falls and head injury may precipitate delirium, although sepsis seems likely in this case.
No.
Seizures may point to a precipitating cause of delirium.
No, I don't think so.
Hallucinations may point toward delirium.
I don't think so.
A prior history of stroke may produce diminished cognitive reserve. However acute stroke is usually the sudden onset of FOCAL neurologic deficit.
No.
Dysthymia may indicate depression rather than delirium.
Well, he usually sleep like a log, but a few nights this week, like last night, he was all confused and worked up and couldn’t rest. Then during the day, when he should be awake, he’s sleepin’.
Disturbed sleep/wake cycle and increased confusion at night are key indicators of delirium.
He's fine with that.
Good thought, urinary incontinence may be a precipitating cause of delirium, and UTI and retention are common in older people. However these seem unlikely in Mr Thomas’ case given the prominent chest symptoms.
Please click on the questions below to obtain Mrs Thomas’s answer. Feedback will also be given in relation to the rationale for asking the question.
He been coughin' a lot....green stuff....hard for him to breathe.
Good start! Use general, open ended questions.
Few months now I reckon, but it got worse in the last week.
This question helps you assess progression and severity of medical condition.
Yeah, him talkin' OK, then he thinks him at home and now he shut up.
Fluctuation is a key feature of delirium.
No. Him talkin' normal before.
An acute change in cognitive function is a key feature of delirium.
Just recently.
To diagnose and distinguish between delirium and dementia it is critical whether condition is acute or chronic.
No. This is the first time he been like this.
Previous history is a risk factor for delirium.
Yes, he have no problem with that.
No, he always know where he's goin'.
This question may eliminate the possibility of a coexisting dementia.
Please click on the questions below to obtain his answer. Feedback will also be given in relation to the rationale for asking the question.
Mr Thomas does not answer or make any eye contact
Begin by seeking permission to gather the history
Mr Thomas does not answer or make any eye contact
It is appropriate to commence with general questions and also to determine the person's level of alertness and engagement.
Although Mr Thomas is unwell, requiring supplemental oxygen, it does seem odd that he will not speak with you at all. Is this just cultural? Although ideally we would seek Mr Thomas' permission before speaking to a relative, this may not be possible in the current situation. It is reasonable to attempt to gather collateral history from Mrs Thomas to try to understand the cause of his current mental state.
Mr Thomas is an independent, cognitively intact 69-year-old Indigenous man living with his wife in the Kalumburu community of WA.
He presented to the community nurse with severe respiratory distress. The RFDS were called to transport Mr Thomas to Perth for urgent assessment and treatment. The transfer team noted Mr Thomas’ oxygen saturation of 91% and suspected right lower zone pneumonia. He was given high flow oxygen, IV ceftriaxone and merepenum and stabilised. His wife accompanied him because of Mr Thomas’ unfamiliarity with urban Australia.
As well as an accurate history of the current presentation it is vital to collect information regarding previous cognitive status, previous functional status, medication use, co-morbid conditions, pain levels, alcohol and drug use and environmental factors in any person presenting with altered mental state.
A diagnosis of CHANGE in mental state can only be made with a good assessment of BASELINE function.

Time's up
Campbell M. Communication with Aboriginal patients in the pre-hospital environment. Australian Journal of Emergency Care 1995;2(2):24-27.
McGrath P, Patton MS., Holewa HG and Rayner RD. The importance of the ‘family meeting’ in health care communication with Indigenous people: findings from an Australian study. Australian Journal of Primary Health 2006; 12(1):56-64
There are some fantastic materials freely available that can assist your learning:
1. Fiona Stanley Hospital Medical Education Unit Delirium Simulation Training Video
The project (click here) was developed locally using Commonwealth Department of Health monies in 2016. The target group is all WA hospital based health workers, including JMOs and Allied Health. All material was field tested and results were presented in a national postgraduate medical conference. It provides you with a great learning resource (23mins46).
2. University of Dundee – Clinical Skills – Delirium Assessment
This video (click here) provides a great (brief; only 7min03) introduction to assessment of an acutely confused person.
Delirium – a guide for nurses – Dr Massarotto
Dementia Delirium in Surgical Patients – Dr Harding
In this interactive case study, you will learn to:
– Recognise and differentiate delirium
– Identify possible predisposing and precipitating causes for delirium
– Apply appropriate tests and assessment skills.
– Treat the symptoms of delirium and its precipitating causes.
– Develop a discharge plan with the patient and family/carer – and its multicultural application.
– Consider utility of multi cultural communication and assessment tools.